There have been a variety of cases over the last couple
weeks, but I will focus on a couple in this post.
Another case that we are currently working on involves a
horse that had a tail wrap applied too tight causing the tissue around the tail
to die. The referring vets tried to
remove the dead parts of the tail in addition to several vertebrae, but were
unable to close the wound fully.
Warning: The following images may be a bit graphic for some people.
The tail was very short on presentation to Brown Equine
Hospital. There was some dirt and
various topical antiseptic agents on the open wound so we clipped and cleaned
the tail and wound to better assess the injury
After cleaning, we could see the wound was a mixture of
necrotic (the black tissue) and granulation tissue (the bright red
tissue).
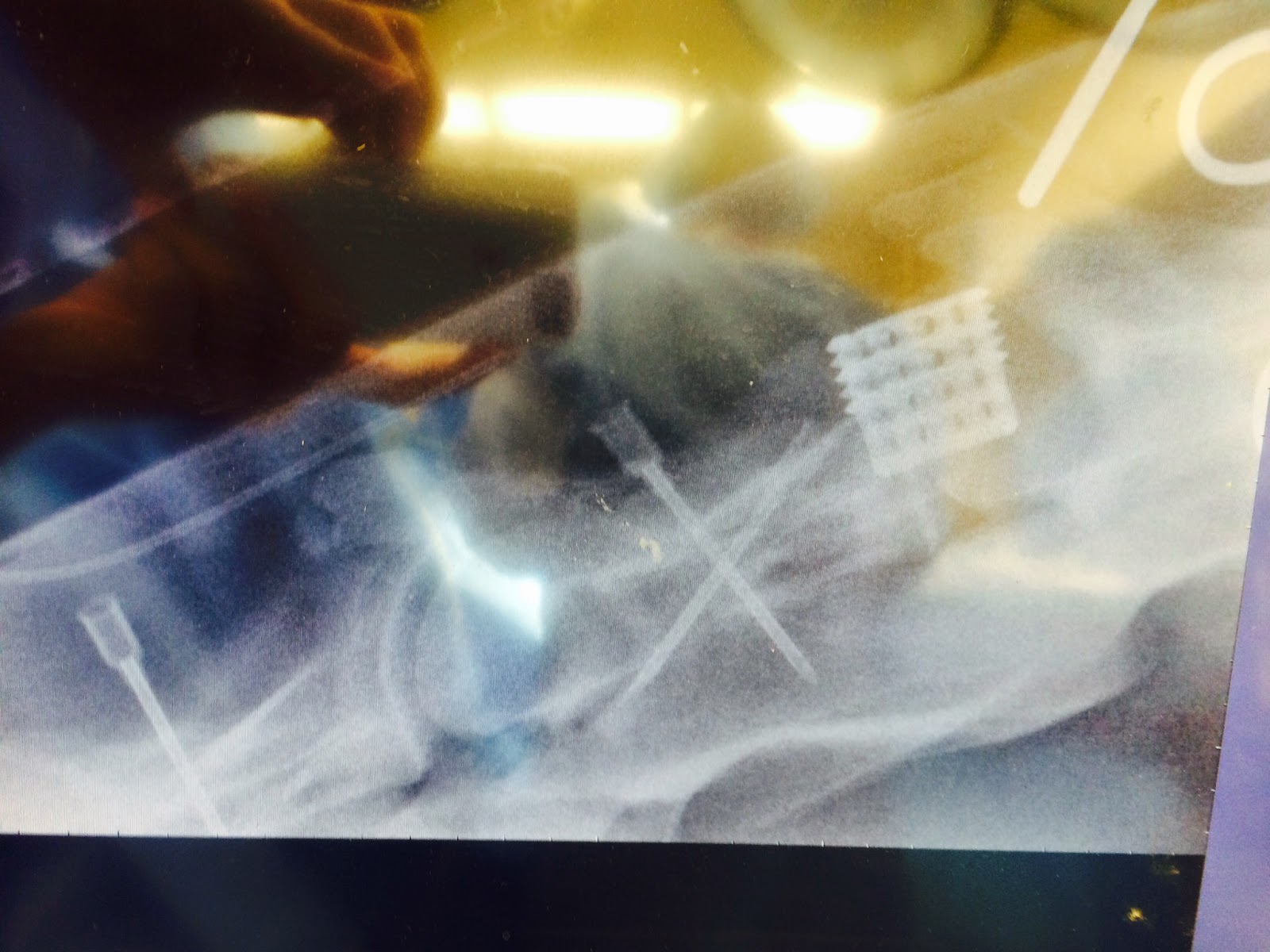
Dr. Hackett and Dr. Younkin removed the remainder of that
vertebrae and a great deal of the granulation tissue in order to have enough
skin to close over the end of the tail.

Closure with a Near-Far-Far-Near suture for tension relief, and then a simple interrupted pattern was placed in between the tension relieving sutures for apposition of the raw edges.
The patient will need to be on systemic antibiotics and
anti-inflammatory drugs for several days to prevent further infection and
minimize pain, but the prognosis for recovery is good!
The next couple weeks will bring several big changes to the
clinic. Dr. Younkin will be finishing
his internship at BEH and heading off to Kansas State for a new position. He has been a valuable source of information
in my first month at BEH and we wish him only the best as he advances in his
career. A new intern who recently
graduated from University of Pennsylvania will be starting next week, and BEH
will also be welcoming a new board certified surgeon to the team from Tufts University,
Dr. Patricia Provost. I am looking
forward to having even more people to learn from!
Until next week!






.jpg)