Hello again from the Bluegrass! As summer winds down here, I
thought I’d take a moment to talk about some of the hard lessons that we learn
in equine/veterinary medicine.
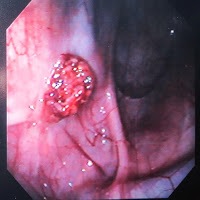
Yesterday started out as a pretty routine day for surgeries
with Dr. Bramlage, but right around 1:00 PM, we had an emergency that came in –
an internal carotid hemorrhage in the right guttural pouch… and when I say
hemorrhage, I mean pouring out! This mare was a 12 y.o. TB mare that had
actually been in sometime between late April and early May with a similar
presentation, and had actually had her internal carotid already ligated
surgically.
Initially when she came in, she left a trail of blood from
the parking lot to a pool in the work-up area and induction stall. Prior to and
during surgery, she had probably lost approximately 20% of her blood volume (so
roughly about 10L – horses have a lot more blood than the average human).
During surgery, she had part of her volume replaced with fluids, Hetastarch,
and plasma, and she was eventually matched with one of the blood donor horses
for a transfusion following surgery. The surgeon on the case performed a
balloon embolization to stop the bleeding from that artery – which,
essentially, puts a “plug” in the vessel by inflating the end of a small,
wire-like catheter with saline (almost like filling a miniature water balloon
that blocks the blood flow).
The surgery was successful at stopping the hemorrhage, and
the mare was placed in the recovery stall and fitted with a blood transfusion
set. Two of the best recovery guys were with her the entire time, and were
extremely conscientious of her condition and how she was progressing. It took a
good hour and a half for her to regain enough strength and come around from
anesthesia to even try to stand up with their assistance – not entirely
unexpected due to how she came in and how long the surgery took (about 3
hours!). The first time, she couldn’t stand up fully, and the team allowed her
to rest in lateral, a.k.a. on her side, a little bit before trying to help her
up again. She was still incredibly weak from all of the fluid she lost and
probably some electrolyte imbalances, etc.
Once she sat up sternal (a.k.a. on her belly), the guys and
an anesthetist adjusted her hooves so that if she tried to stand again, she
would be in a better position for success. Again, she tried to stand with their
assistance, but, she was still too weak and collapsed from fatigue – this time,
it was not a smooth fall. To everyone’s dismay, when she collapsed, she also
completely fractured her right tibia (for all you basketball fans, think Kevin
Ware in the NCAA tourney). Tibial fractures in horses are basically fatal
because they cannot be easily repaired without major complications. And, fractures
during recovery are every veterinarian’s worst nightmare.
When this happened, the interns sprung to action and were
able to sedate her until her owners could be reached, and quite regrettably,
she was euthanized. No one was truly to blame in this situation, nor did anyone
expect for this to happen. It’s just one of the unfortunate and undesirable
things about equine surgery. Mostly, I feel for the surgeon and the intern on her
case – it’s devastating to complete a difficult, 3-hour-long surgery and have a
positive outlook for your patient, and then have something so tragic happen
that absolutely no one could control.
So, this blog is in memory of the sweet mare that we lost, though
please do not let it scare you – fractures during recovery are rare if the
recovery team is good at what they do, and they should never be anticipated as
though it will inevitably happen. Props to our recovery guys, who watch out for
the safety of all surgery patients each day, and even risk their own safety for
many of our horses!