Well, it has finally sunk in that my time with the MSU
Equine Summer Fellowship Program and Brown Equine Hospital has come to an end.
I could not have imagined a better experience and I would do it all over again
in a heartbeat. The vets and techs at Brown Equine Hospital taught me so much
and were so supportive, I could not ask for a better group of people to work
with. I was very sad to say goodbye, but I left with many fond memories. So
here it is, my final blog post:
Something must have been in the air this week, because we
received four emergency colic cases in less than three days. The first to be
brought in was a draft horse that had been off feed since the night before.
From the abdominal ultrasound and rectal exam, Dr. Brown diagnosed him with anterior
enteritis, or inflammation of the duodenum and/or jejunum. Since anesthetizing
draft horses carries an even higher risk than other horses, Dr. Brown wanted to
keep this gelding off the table at all costs. We started by passing a
nasogastric tube to reflux every few hours and administering IV fluids with a
lidocaine drip. The draft horse took a turn for the worst a couple days into
treatment, refluxing up to 30 liters and going into acute renal failure. We
increased the frequency of refluxing and started to bolus the IV fluids.
Remarkably, the gelding pulled through and is now recovering well. We stopped
refluxing completely and have started weaning him back onto solid food.
The second colic that came in was a part-Standardbred that had
been acting uncomfortable for a couple days. As it turned out, this gelding also
had anterior enteritis and we started him on the same treatment regimen as the
draft horse. Unfortunately, our refluxing did not keep pace with the fluid
backing up into his stomach. About 48 hours after being admitted, we passed a
tube, but we got negative net reflux. Suspicious, Dr. Brown performed another
ultrasound and belly tap. The results showed excessive fluid (reflux)
surrounding the intestines, revealing that the gelding’s stomach had ruptured.
Sadly, we had to put the horse down. It is surprising how such similar cases,
treated the same, can end so differently.
The last two cases were also treated medically. An impaction
and a right dorsal displacement were resolved with IV fluids and fasting. Both
horses were slowly reintroduced to solid food and were sent home within two
days of being admitted. I had always thought that all colic cases that were
referred went to surgery. Much to my surprise, however, the vast majority of
the colic cases we saw this summer were treated and resolved medically. Another
surprise was how many of the horses that came in for colic went home healthy;
it was nice to discover that colic is not a death sentence.
To end, here are a few photos of some of my favorite moments
working at Brown Equine Hospital:
Repro work with Dr. Jen Brown
Surgery with Dr. Keith Brown
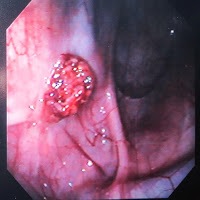
Scoping with Dr. Travis Tull